When and Why to Outsource Your Institutional Biosafety Committee
Author: Zoë Worthington
All clinical studies require review by an Institutional Review Board (IRB) to protect patients and ensure the study is conducted ethically. In recent years, the use of gene therapy to combat various diseases has expanded dramatically. This type of research uses recombinant or synthetic nucleic acid molecules (r/sNA) which requires special handling and additional review by an Institutional Biosafety Committee (IBC).
IBCs play a fundamental role in ensuring the safe and responsible use of any biological agents in gene therapy research and development. The IBC reviews proposals for the use of hazardous biological materials, conducts risk assessments, provides guidance on biosafety and biosecurity best practices, and more.
Whether you are new to the concept of IBC review or have previous experience in this area, understanding what an IBC does, when and why IBC review is required, and the potential benefits of outsourcing your IBC services is critical.
What is an Institutional Biosafety Committee?
An Institutional Biosafety Committee (IBC) is an institution-specific panel of experts who review and oversee work with recombinant material, such as human gene therapy products, that have specific biosafety requirements for storage, safe handling, administration, and disposal.
An IBC consists of at least five members, including a biosafety professional, representatives from your institution or organization, and two local members who are not associated with your organization. The main responsibility of the IBC is to ensure that all aspects of the guidelines set by the National Institute of Health (NIH) are met and the risks involved in handling the recombinant material are assessed in an independent manner.
Depending on the nature of the research being reviewed, the committee will also include an expert in human gene therapy, animal containment, and/or plant research. IBCs can be formed in-house by the institution, or an external IBC can be used formed by an independent body outside of an organization.
Why are Institutional Biosafety Committees Important?
The most important role of an IBC is to ensure that clinical research using r/sNA (or potentially other hazardous agents) is conducted in a manner that is safe for research staff and the surrounding community. Investigational agents involving r/sNA are very different from other treatments and medications typically used in clinical research and have specific handling requirements.
Compliance with the NIH Guidelines is a central tenet for all IBCs, whether the IBC is formed internally or externally. Their purpose is to ensure that these guidelines are met while minimizing the potential for inappropriate handling of biohazardous materials, funding loss, or delays due to non-compliance. IBC oversight continues for the duration of the study ensuring that the site remains compliant regardless of any changes in the study that may occur.
It is important to note that for an IBC to be effective, it must have a comprehensive understanding of the potential hazards associated with biological agents and the resources necessary to manage these risks. This is achieved by completing sufficient documentation to allow the IBC members to understand the nature of the investigational agent and how it will be handled at your institution, from receipt to eventual disposal.
What Requires Institutional Biosafety Committee Review?
If your study or institution receives funding from the NIH and involves the use of r/sNA, the NIH Guidelines require you to form an IBC to review the work periodically. The IBC is responsible for reviewing at a local level and overseeing this research until its conclusion. For clinical studies, IBC approval must be obtained before the research or study can begin for any work that involves recombinant material. Common recombinant materials include, cell and gene therapy products and mRNA vaccines.
While IBCs are focused on research involving r/sNAs, they can have oversight over any research if an institution desires. Regardless of where an institution receives funding, it is considered best practice to have an IBC oversee research with potential biosafety implications.
IBC oversight always continues until the study is closed and the investigational agent is off site. Typically, studies are reviewed annually, however, changes (made either by the investigator, institution, or by study sponsors) must be reviewed by your IBC and may necessitate additional meetings depending on the modifications.
Key Benefits of Outsourcing your Institutional Biosafety Committee
Whether you are new to this process or already have an in-house IBC, there are significant benefits to using an external IBC service provider. For most institutions the main reason to use external IBC services is reducing the time for study start-up and IBC approval.
Often, in house IBCs only have the bandwidth to meet monthly or at greater intervals and typically review studies in batches, which could mean a delay in reviews. External IBCs can typically meet on an as needed basis for example, as soon as a site is ready. This also allows the clinical team to focus on other pressing needs such as maximum enrollment requirements, etc. during study start up. Other key benefits that an external IBC can provide include:
- Reducing the workload for busy staff and expediting review
- Eliminating common mistakes that delay approval and maximizing success
- Creating a smooth and frustration free process
- Providing fast access to a pool of IBC members
- Gaining highly-trained biosafety expertise not normally found in smaller institutions
- Delivering transparency and objective expert evaluation of your biosafety program
- Offering guidance for reporting to the NIH
Sitero’s External Institutional Biosafety Committee Services
Sitero’s IBC experts have extensive experience helping sites prepare their facilities for any study requiring or wanting IBC review, as well as forming and registering our customer’s IBC with the NIH. Getting ready for review requires many documents to explain how and where the investigational agent will be handled at your institution and the collection of equipment information and certification (e.g., Biological Safety Cabinet). Additionally, our experts understand what preparations can occur simultaneously which helps maximize time usage.
As an external IBC, Sitero has access to a broad network of experienced subject matter experts who can be resourced to form an IBC for your study. Preparing for IBC review is complex and time-consuming. Outsourcing IBC services can streamline the process, not only for your first study, but can also ensure that subsequent projects will be better prepared as common documentation can often be shared.
Conclusions
Outsourcing IBC services can be incredibly impactful for organizations of any size. Utilizing an external IBC provider can allow you to expedite the review of your study, significantly shortening time to start up, all while lightening the load for your staff and ensuring compliance to NIH Guidelines. When you use external IBC services, your researchers can spend time on their research rather than administrative tasks and still be involved in the review process as desired. Importantly, the added layer of transparency with an external committee provides an even more independent review.
Sitero provides comprehensive IBC services, however, we also offer a la carte service options. For example, Sitero’s external IBC experts are available to support your established biosafety committee by providing additional expertise, conducting risk assessments, aiding in setting up or improving your biosafety program, and/or coordinating the review process. Our external IBC services can provide as little or as much support as you need to ensure that your IBC functions at its most safe and efficient. Contact us to learn more.
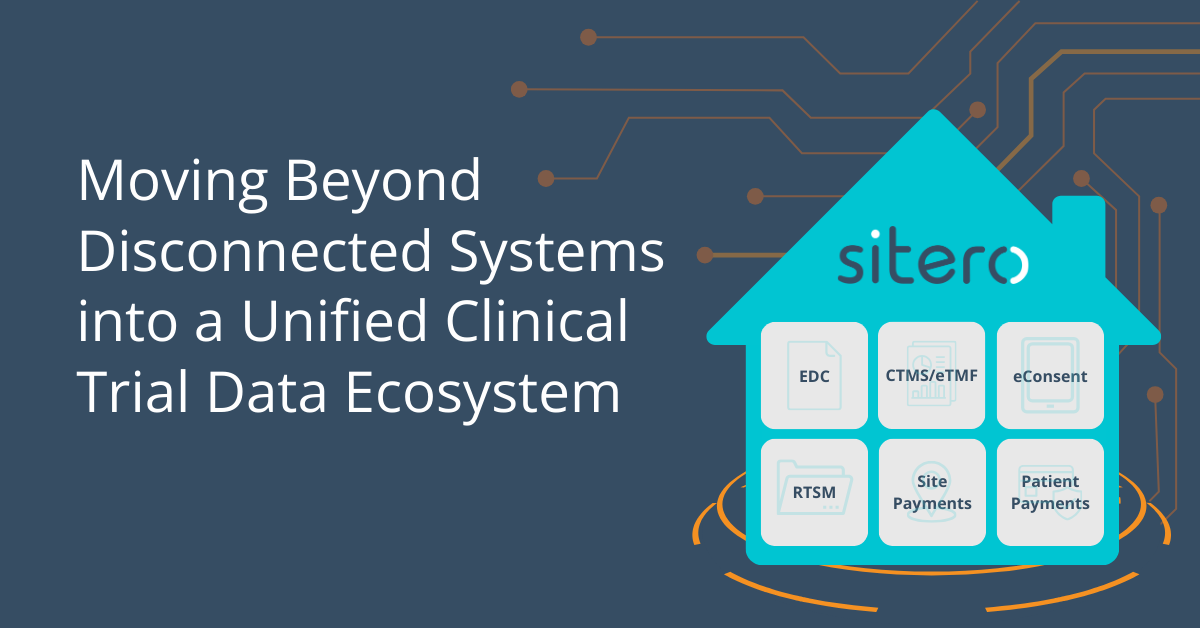
The future of clinical trials is a unified, interoperable ecosystem. Sitero’s Mentor platform is leading this transformation, ensuring that clinical trials are more efficient, compliant, and streamlined than ever before. Learn more in our latest blog:
Today’s trials require data entry from anyone, anywhere including patients, sites, home nurses, and remote investigators. Learn why EDC systems must evolve to support decentralized trails in our latest blog: