The Power of Electronic Data Capture (EDC) Systems in Clinical Research
In the world of clinical research, efficiency, accuracy, and data integrity are paramount. With the advance of technology, traditional paper-based methods of collecting and managing clinical data have given way to Electronic Data Capture (EDC) systems. These tools have revolutionized the way clinical research is conducted, offering numerous advantages that enhance the entire research process.
What are Electronic Data Capture (EDC) Systems?
EDC systems are digital platforms designed to collect, manage, and store clinical trial data electronically. They serve as comprehensive solutions that replace cumbersome paper-based methods, facilitating the collection and analysis of data throughout the entire research lifecycle. EDC systems are highly customizable, allowing researchers to tailor data capture forms, validation rules, and workflows to suit the specific needs of their studies.
These systems streamline the process of data collection by providing a centralized and secure platform where researchers, clinicians, and other stakeholders can input and access information in real-time. EDC systems often include features such as automated data validation, which helps identify errors or inconsistencies during data entry, reducing the likelihood of inaccuracies, they enhance the efficiency of clinical trials by enabling remote monitoring, facilitating faster data review, and allowing for prompt decision-making.
Furthermore, EDC systems contribute to the overall quality and integrity of clinical trial data. They offer audit trails and version control, ensuring a transparent and traceable record of all data modifications and updates. This not only supports regulatory compliance but also enhances the credibility of research outcomes. Overall, EDC systems play a crucial role in advancing the efficiency, accuracy, and security of data in clinical research, ultimately contributing to the progress and the development of new treatments and therapies.
Why is EDC Important?
EDC is crucial in the realm of clinical research due to its transformative impact on the management of data. The shift from paper-based to electronic systems significantly enhances efficiency by allowing real-time data entry and validation. This not only expedites the data collection process but also minimizes errors, improving the overall accuracy of the collected information.
EDC systems are highly adaptable, enabling researchers to customize data capture forms and workflows according to the specific requirements of their studies, promoting flexibility and tailored solutions. All while maintaining data in standard and compatible formats for export, consistent with statistical software for the analysis process.
Beyond efficiency, EDC systems play a pivotal role in ensuring data security and compliance. In an era where data integrity and participant privacy are paramount, EDC systems provide a secure digital environment for storing and managing sensitive information. With built-in encryption, access controls, and audit trails, these systems mitigate the risk of unauthorized access and data breaches, aligning with stringent regulatory standards. The importance of EDC in maintaining the confidentiality, reliability, and traceability of clinical trial data makes it an indispensable tool for advancing medical research and drug development.
Key Benefits of EDC Systems
EDC systems play a pivotal role in clinical trials and research by offering a myriad of benefits. They streamline the process, replacing traditional paper-based methods with digital platforms that offer real-time data entry, validation, and customization.
EDC systems enhance efficiency, reduce errors, and contribute to the overall quality and integrity of clinical trial data. With features like remote monitoring and audit trails, these systems promote quicker decision-making, regulatory compliance, and transparency, ultimately accelerating the pace of research and improving the reliability of outcomes in the healthcare and pharmaceutical fields. Some key benefits include:
- Data Accuracy: EDC systems significantly reduce the risk of data entry errors compared to manual paper-based methods. These systems often include built-in validation checks, reducing the likelihood of inconsistencies and ensuring data accuracy.
- Real-time Monitoring: Researchers and sponsors gain real-time access to study data, allowing for continuous monitoring and early detection of potential issues. This enables faster decision-making and intervention if necessary.
- Efficient Data Collection: EDC systems streamline data collection processes by providing electronic forms that are easy to complete and validate. This enhances participant engagement and reduces the time required to collect complete and reliable data.
- Remote Data Entry: EDC systems support remote data entry, allowing study participants to submit data from different locations. This is particularly valuable in long-term or decentralized trials, improving convenience for both researchers and participants.
- Analysis: EDC systems facilitate data exports in standard and compatible formats consistent with statistical software, streamlining the analysis process.
- Data Security and Compliance: EDC systems offer robust data security features, including role-based access controls and audit trails. These measures ensure data integrity, confidentiality, and compliance with regulatory requirements.
- Centralized Data Storage: Unlike paper-based methods, EDC systems centralize data storage, making it easier to retrieve, analyze, and share data with stakeholders such as regulatory authorities, ethics committees, and collaborators.
Stages of EDC in Clinical Research
EDC typically involves distinct stages. Initially, the system is configured to align with the specific requirements of the study, including the design of electronic case report forms (eCRFs) and the establishment of data validation rules. The next stage encompasses data collection, where researchers and clinicians input information directly into the EDC system in real-time.
Subsequently, data cleaning and validation occur, addressing any discrepancies or errors through systematic checks. The final stage involves data analysis and reporting, leveraging the consolidated and standardized data stored in the EDC system to draw meaningful insights and conclusions, ultimately contributing to the advancement of therapeutic development.
- Protocol Development: Researchers can design electronic case report forms (eCRFs) tailored to the study protocol, capturing the specific data points required for analysis.
- Data Collection: Participants enter data directly into the EDC system, eliminating the need for paper-based diaries or questionnaires.
- Monitoring: Real-time access to data allows researchers to monitor study progress and detect anomalies promptly.
- Quality Control: EDC systems often include built-in data validation checks that ensure the accuracy and completeness of collected data.
- Statistical Analysis: EDC systems facilitate data export in formats compatible with statistical software, streamlining the analysis process.
- Regulatory Submissions: The organized and secure data stored in EDC systems aids in preparing regulatory submissions and responding to inquiries.
Conclusions
In conclusion, EDC systems have transformed the landscape of clinical research by improving data accuracy, efficiency, and overall study quality. As technology continues to advance, these systems are likely to evolve further, offering even more features that enhance the research process and contribute to the development of safe and effective medical treatments.
Sitero’s EDC suite of products provides a range of services that enable sponsors and CROs to get exactly the level of support they need to eliminate obstacles, operate more efficiently, and easily manage data for a single study or a global portfolio of clinical trials – all using a single, powerful, proven platform that combines deep EDC experience with impressive ease-of-use to put everything they need at their fingertips. Contact us to learn more about our Mentor EDC solutions.
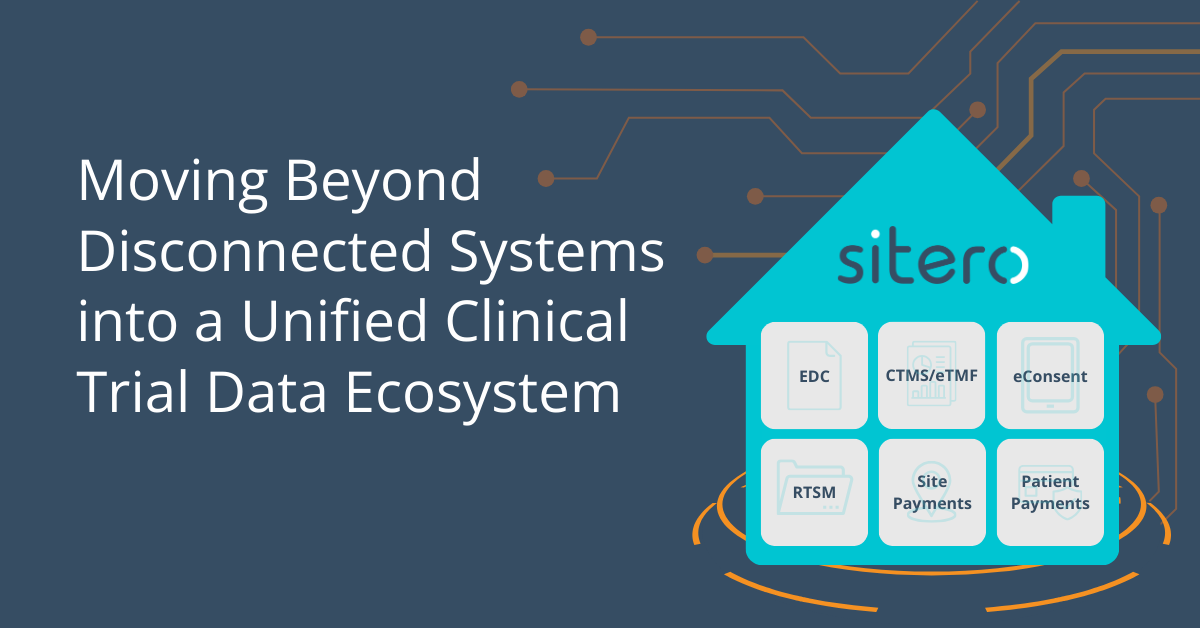
The future of clinical trials is a unified, interoperable ecosystem. Sitero’s Mentor platform is leading this transformation, ensuring that clinical trials are more efficient, compliant, and streamlined than ever before. Learn more in our latest blog:
Today’s trials require data entry from anyone, anywhere including patients, sites, home nurses, and remote investigators. Learn why EDC systems must evolve to support decentralized trails in our latest blog: